Introduction to Digital MHPSS
Advantages of Digital MHPSS
Using digital methods can help us reach more people and be more inclusive in the growing MHPSS area. The increased availability of Internet and mobile technologies coupled with the potential effectiveness of low-intensity psychological interventions provides opportunities to offer MHPSS services to a wide range of individuals.
Compared to face-to-face services, the spectrum of digital psychological and psychosocial support offers the following advantages:
Safety
Digital interventions prevent experiences of stigmatization and thus reduce barriers to seeking psychological and psychosocial help by enabling anonymous, non-public and secure use.
Scalability
With digital interventions, MHPSS efforts can be diversified and larger parts of the population can be reached with fewer human and financial resources.
Digital interventions have the potential to improve access for geographically remote areas and can reduce barriers such as transportation costs, lack of free time, lack of childcare or fear of stigmatization.
Sustainability & Participation
With digital technologies broad-scale interventions that allow representation and community participation can be created. Content and design can be continuously adapted and contextualized to the needs of the target group with a participatory approach and be delivered to the users through appropriate channels. Once the technology is in place, the variable costs of digital interventions are low.
Effectiveness
Over 300 studies from 20 years of research show, that technology-empowered and internet-based mental health services are an effective, resource-efficient extension of face-to-face approaches care.
Challenges with Digital MHPSS
Besides these advantages, there are, however, also critical aspects that need to be considered when choosing digital pathways to MHPSS:
Safety
- Digital MHPSS interventions may fall short in delivering effective crisis care.
- Rapid action in situations of acute, especially suicidal situations is limited due to the lack of contact and anonymous use.
- Digital MHPSS services may further cause unintended harm to users when misused, when the provided information is outdated or when employed in contexts where MHPSS is highly stigmatized.
- Concerns of intruding privacy and protect data have been expressed in the development of new technologies.
Scalability
- Access to digital services can be limited due to structural, social, or individual barriers.
- A primary concern is the lack of internet coverage and/or end devices.
- Service users might not have sufficient privacy within their homes to confidentially access MHPSS services, especially because mental health issues are often highly stigmatized
- The use of digital MHPSS services requires a high level of motivation, a relatively high level of digital literacy and affinity, and minimum reading/ writing skills on the part of the users.
Sustainability & Participation
- Interventions that are app- or web-based require updates to improve user experience, warrant data protection, update information, and comply with changing regulations. This requires long-term and continuous staff time and thus financing.
- A lack of structural embedment of the digital MHPSS service in the existing health system also prevents a long-term and sustainable implementation.
- Involving many different stakeholders and target group representatives requires time, resources, patience and flexibility.
Effectiveness
- Evidence is often from Western, educated, industrialized, rich (WEIRD) countries
- Evidence is mainly related to specialized mental health interventions, while there is a gap in the literature regarding the effectiveness of digital basic psychosocial support.
- For a positive impact of digital MHPSS a consistent use of the recommended program is essential: Their effectiveness can be restricted due to a lack of incentives, relevance, control of use or fit with the target group’s context of life.
Categorization of digital MHPSS services
Digital MHPSS services can differ according to the form of use, the extent and form of contact resp. in the degree of automation and the phase of the intervention.
Forms of use
-
Information
– Psychoeducation about diseases and treatment options
-
Communication
– Forums
– E-mail
– Chat
– Phone/video call
-
Intervention
– Prevention
– Self-help
– Treatment
– Aftercare
Contact: form and extent
-
Unguided or self-guided
- Web-based self-help programs without contact to a professional or lay person (e.g. peer support)
-
Guided or supported
- Short online contacts with a professional or a trained lay person
- Little contact compared to face-to-face services
-
Face-to-face service but via e-mail, chat or video
- Support from professionals comparable to face-to-face services
- Require a similar amount of time as face-to-face services
- Communication can happen simultaneous/synchronous or delayed/ asynchronous
–
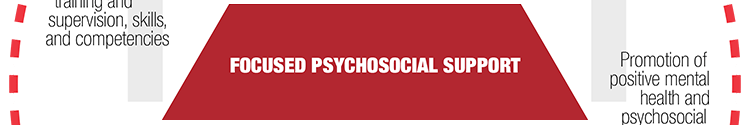
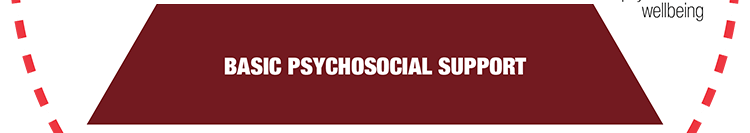
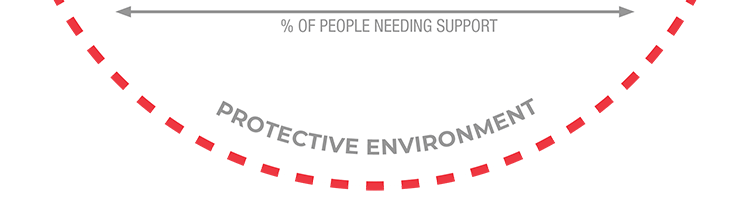
Level of intervention
The MHPSS pyramid describes services on four different levels of specification. Digital services can be used on every level as e.g., digital self-care, focused support groups or technology-supported in-person treatments. It is important to determine at the beginning which target group with which needs is to be reached and to select the level of intervention accordingly.